Dry Eye Syndrome
If you suffer from chronic dry eye, redness, irritation and fatique with reading and/or computer use, you may have Keratoconjunctivitis Sicca, or Dry Eye Syndrome. Using different tests, our doctors can diagnose and prescribe therapy for Dry Eye Syndrome. Depending on the type and severity, it may range from simple eye exercises to ocular lubricants to punctual occlusion.
What is Dry Eye Syndrome?

Dry eye syndrome (Keratoconjunctivitis Sicca) is the result of an inflammatory process affecting both the lacrimal gland (the gland that produces tears) and the surface of the eye. As a result, people who suffer from dry eye syndrome have either reduced tear production or excessive tear drainage. This causes discomfort and can damage the surface of the eye. Symptoms may include dryness, stinging, burning, itching, scratchiness, excessive tearing, blurry vision, and sensitivity to light.
Citing U.S. figures, more than 10 million people in the U.S.A. suffer from moderate to severe dry eye syndrome, and an estimated 15 to 20 million have a milder form of the condition. Nearly 5 million people are unable to wear contact lenses because of dry eye.
Dry eye can affect men and women of any age. At particular risk are those who:
While there is no known "cure" for dry eye, it can be often be managed with an artificial tear solution or, in more severe cases, by blocking the puncta. Whatever the treatment mode chosen, effective treatment of dry eye must either replace, enhance or retain natural tears.
To replace natural tears, an artificial tear solution can be effective. Artificial tears are available with and without preservatives. Preservative-free artificial tears are recommended for people who can’t tolerate preservatives or who must use these solutions many times per day.
If artificial tears are needed on more than an occasional basis, the type of preservative used is an important consideration. Many artificial tear solutions contain benzalkonium chloride (BAC), a preservative that with frequent use can actually damage the epithelium and lead to further problems.
To enhance natural tears, a more advanced artificial tear is required. Such solutions would include artificial tears with formulations containing zinc and bicarbonate, substances that can actually contribute to the growth and maintenance of healthy mucin, tear film, and epithelium. Often, overnight protection is needed. In these cases a more viscous preparation should be used, one that is designed to provide long-lasting protection and lubrication.
To retain natural tears, it is necessary to suppress the loss of tears by blocking the punctum (the natural drain for tears). This is done with the insertion of punctal plugs that actually block the opening of the punctum.
Plugs made for smooth insertion, comfortable wear and virtual invisibility are the most popular. In more severe cases, patients may need to be treated with eyelid inserts, tear duct plugs, protective glasses, bandage contact lenses or surgical procedures.
Citing U.S. figures, more than 10 million people in the U.S.A. suffer from moderate to severe dry eye syndrome, and an estimated 15 to 20 million have a milder form of the condition. Nearly 5 million people are unable to wear contact lenses because of dry eye.
Dry eye can affect men and women of any age. At particular risk are those who:
- Wear contact lenses
- Are Computer Users
- Are pregnant
- Are on specific types of medication
- Are post menopausal
- Have suffered external eye diseases
- Have Sjogren’s syndrome
- Have had PRK or LASIK
- Have Scleroderma
While there is no known "cure" for dry eye, it can be often be managed with an artificial tear solution or, in more severe cases, by blocking the puncta. Whatever the treatment mode chosen, effective treatment of dry eye must either replace, enhance or retain natural tears.
To replace natural tears, an artificial tear solution can be effective. Artificial tears are available with and without preservatives. Preservative-free artificial tears are recommended for people who can’t tolerate preservatives or who must use these solutions many times per day.
If artificial tears are needed on more than an occasional basis, the type of preservative used is an important consideration. Many artificial tear solutions contain benzalkonium chloride (BAC), a preservative that with frequent use can actually damage the epithelium and lead to further problems.
To enhance natural tears, a more advanced artificial tear is required. Such solutions would include artificial tears with formulations containing zinc and bicarbonate, substances that can actually contribute to the growth and maintenance of healthy mucin, tear film, and epithelium. Often, overnight protection is needed. In these cases a more viscous preparation should be used, one that is designed to provide long-lasting protection and lubrication.
To retain natural tears, it is necessary to suppress the loss of tears by blocking the punctum (the natural drain for tears). This is done with the insertion of punctal plugs that actually block the opening of the punctum.
Plugs made for smooth insertion, comfortable wear and virtual invisibility are the most popular. In more severe cases, patients may need to be treated with eyelid inserts, tear duct plugs, protective glasses, bandage contact lenses or surgical procedures.
Blepharitis
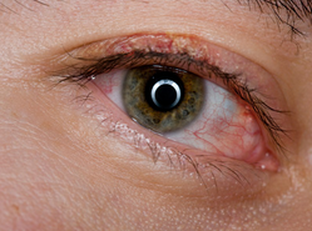
Blepharitis is an inflammation of the eyelids. Redness, swelling, styes, cysts, and flaky crusts at the eyelid margin characterize it. Symptoms include scratchy, swollen, burning, itching, tender and irritated eyes. Blepharitis can be caused by various bacteria and be chronic or acute in presentation. People with skin conditions such as rosacea, acne, and eczema are more prone to have blepharitis flare ups. Poor facial hygiene can also be a contributing factor.
An eye doctor will diagnose the specific type of blepharitis during an eye exam. Treatment options are abundant and include over the counter remedies and prescription eyedrops and ointments. Occasionally, minor eyelid surgery is necessary to remove cysts when topical treatments are unsuccessful. Blepharitis, in some cases, requires ongoing treatment along with eyelid hygiene to maintain eye comfort and appearance.
An eye doctor will diagnose the specific type of blepharitis during an eye exam. Treatment options are abundant and include over the counter remedies and prescription eyedrops and ointments. Occasionally, minor eyelid surgery is necessary to remove cysts when topical treatments are unsuccessful. Blepharitis, in some cases, requires ongoing treatment along with eyelid hygiene to maintain eye comfort and appearance.
Cataracts
The crystalline lens located behind the eye's iris is normally clear and helps to focus light and images entering the eye onto the retina in the back of the eye. A cataract is the clouding of the crystalline lens, preventing the light from properly focusing on the retina. Cataracts usually occur naturally with age but can also be caused by ocular trauma, exposure to UVA light, health conditions such as diabetes, some medications such as steroids, or they can be developed at birth. Cataracts can occur in one or both eyes and does not spread from one eye to the other like an infection. Most cataracts develop very slowly over time, gradually causing blurred vision, decreased color contrast, increased glare or halos around lights, and frequent changes in glasses prescriptions.
|
There are no medications that can prevent or slow the progression of cataracts. Once a cataract begins to affect your vision and hinder your daily lifestyle, the lens can be removed and replaced with a simple outpatient procedure that usually takes only 10-15 minutes. Cataract surgery does not usually require needles or stitches, and is a quick and painless procedure.
|
Diabetic Retinopathy
The most common diabetic eye disease is diabetic retinopathy, which is a leading cause of blindness in American adults. In some people with diabetic retinopathy, the tiny blood vessels within the eye can swell and leak, or new blood vessels can develop and grow on the surface of the retina. In many cases, this abnormal growth or leaking can cause permanent damage to the retina, so it is important to detect any changes in your retina at an early stage and prevent any permanent loss of vision. Anyone with diabetes is at risk of developing this condition, and approximately 45% of Americans with diabetes have some stage of retinopathy.
|
Some diabetic retinopathy may not present with any noticeable symptoms at first. Over time, as the condition worsens, you may notice dark spots floating in your vision, which is usually a sign of blood leaking from the vessels. These hemorrhages tend to happen more than once, and often while sleeping. If you notice any of these sudden spots in your vision or quickly develop blurred vision, contact your eye care professional immediately before more bleeding occurs. The earlier you receive treatment, the more likely treatment will be effective.
|
Floaters
You may occasionally notice tiny specks that float about in your vision, usually small, shadowy shapes that can look like strands of thread or even amoebas. They often move as your eyes move and can dart away when you try to look at them, slowly drifting when your eyes stop moving. These are referred to as "floaters" and are familiar to most people.
Floaters usually become noticeable when looking at something bright or when in bright environments. They normally occur when the vitreous (the gel-like substance that fills the eye) begins to clump and condense with age. The stringy, shadowy specks you often see are the shadows cast onto the retina from these clumps. In most cases, floaters are simply a nuisance, but if you notice a sudden increase in the number of floaters or if they are accompanied by flashes of light or a veil of shadows in your vision, contact your eye care professional immediately. These symptoms may be a sign of a more serious condition such as diabetic retinopathy or a retinal detachment.
Floaters usually become noticeable when looking at something bright or when in bright environments. They normally occur when the vitreous (the gel-like substance that fills the eye) begins to clump and condense with age. The stringy, shadowy specks you often see are the shadows cast onto the retina from these clumps. In most cases, floaters are simply a nuisance, but if you notice a sudden increase in the number of floaters or if they are accompanied by flashes of light or a veil of shadows in your vision, contact your eye care professional immediately. These symptoms may be a sign of a more serious condition such as diabetic retinopathy or a retinal detachment.
Glaucoma
Often referred to as "the silent thief of sight," glaucoma is a potentially blinding condition if left untreated. Glaucoma is a disease that damages the optic nerve, which is the connection between the eye and the brain. Glaucoma has been associated with high eye pressure, which is why all doctors check eye pressure at every exam. However, glaucoma can also occur if you have normal eye pressure. Having increased eye pressure does not necessarily result in developing glaucoma, but it does put you more at risk. People who have a family history of glaucoma are at the highest risk, but other factors can contribute to the risk including ethnicity and age.
Glaucoma may not have any noticeable symptoms at first, but as the disease progresses, persons with glaucoma may notice their side vision beginning to blur or disappear. Eventually, if left untreated, they will slowly lose their peripheral vision and develop "tunnel vision." Over time, central vision will also become affected and decrease until no vision remains.
Glaucoma may not have any noticeable symptoms at first, but as the disease progresses, persons with glaucoma may notice their side vision beginning to blur or disappear. Eventually, if left untreated, they will slowly lose their peripheral vision and develop "tunnel vision." Over time, central vision will also become affected and decrease until no vision remains.
|
Glaucoma can be detected through a number of tests and procedures performed during a comprehensive eye exam. Your doctor should check your eye pressure, your visual acuity to determine how well you see at various distances, as well as your peripheral vision. A dilated eye exam or retinal photography should be performed to examine the health of the optic nerve and surrounding tissues. Determining the thickness of your cornea through a simple test called pachymetry is also helpful in determining your risk of glaucoma. Often, Dr. Granek will perform a visual field test to check peripheral vision.
|
Glaucoma cannot be cured, but when detected early most glaucoma can be well managed with daily eye drops. Unfortunately the need for drops is permanent and does not work for all people, in which case surgery may be necessary. Regular visits to your eye care professional are required to monitor the progression of glaucoma and determine if any changes to treatment are needed.
Macular Degeneration
Age-related Macular Degeneration (AMD) is the most common cause of legal blindness among people over the age of 60. AMD is a disease that affects the area of central vision in the retina called the macula. There are two types of AMD: wet or dry.
Wet AMD occurs when abnormal blood vessels behind the retina begin to grow beneath the macula, leaking fluid and blood that raises the macula. This type of AMD causes rapid vision loss and will often cause straight lines to appear wavy and distorted. This type of AMD needs immediate attention.
Dry AMD is more common and occurs when cells in the macula begin to break down and deteriorate, leaving yellow deposits called drusen under the retina. This causes blurred central vision which can develop into a dark spot over time, eventually blocking all central vision. Early signs of dry AMD may include blurred central vision, difficulty recognizing people's faces, or requirng more light for reading and other tasks. Dry AMD can eventually or suddenly turn into wet AMD, even during the early stages. Once dry AMD reaches the advanced stage, no form of treatment can prevent vision loss. However, treatment can delay and possibly prevent progression, so early detection is important.
Wet AMD occurs when abnormal blood vessels behind the retina begin to grow beneath the macula, leaking fluid and blood that raises the macula. This type of AMD causes rapid vision loss and will often cause straight lines to appear wavy and distorted. This type of AMD needs immediate attention.
Dry AMD is more common and occurs when cells in the macula begin to break down and deteriorate, leaving yellow deposits called drusen under the retina. This causes blurred central vision which can develop into a dark spot over time, eventually blocking all central vision. Early signs of dry AMD may include blurred central vision, difficulty recognizing people's faces, or requirng more light for reading and other tasks. Dry AMD can eventually or suddenly turn into wet AMD, even during the early stages. Once dry AMD reaches the advanced stage, no form of treatment can prevent vision loss. However, treatment can delay and possibly prevent progression, so early detection is important.
|
Risk factors associated with macular degeneration include smoking, obesity, race (Caucasians are much more likely to develop AMD), family history, and gender (women appear to be at greater risk than men). Eating a healthy diet high in antioxidants (such as green leafy vegetables and fish), not smoking, maintaining normal blood pressure, exercise, and weight management can all play a role in reducing your risk of AMD.
|
Myopia
Nearsightedness, called myopia, occurs when the overall shape of the eye is longer in length than the normal eye. This causes light rays to come to a focus somewhere in front of the retina, causing blurred vision of distant objects while objects up close are clearer. There are different degrees of myopia from minimal to extreme, and can often occur with astigmatism and/or presbyopia.
Hyperopia
Farsightedness, called hyperopia, occurs when the overall shape of the eye is shorter in length than the normal eye. This causes light rays to come to a focus somewhere behind the retina, causing blurred vision of nearby objects and sometimes distant objects as well, depending upon the amount of hyperopia. Farsightedness is different than presbyopia (the need for reading glasses after age 40) and can occur with both astigmatism and presbyopia at the same time.
Astigmatism
Astigmatism is blurry and distorted vision caused by an eye that is not perfectly shaped. In an ideal eye, the front clear surface of the eye would be spherical and focus light and images into a single point inside the eye. In an eye with astigmatism, the front of the eye has a more cylindrical shape, and so light passing through that surface becomes blurred and distorted. Astigmatism is present in most people and most astigmatism can be corrected with glasses, contacts, or vision surgery. Astigmatism usually occurs with myopia (nearsightedness) or hyperopia (farsightedness).
Presbyopia
Presbyopia is a condition that eventually affects 100% of people and is usually first noticed in our early 40's. The crystalline lens inside the eye is responsible for our ability to change the focus of our eyes. When we are young, the lens is very flexible and can focus on distant objects or very near objects. By the time we are in our early 40's, the lens is much less flexible and is not able to focus on near objects, which is why people begin holding reading material further away or begin wearing reading glasses or bifocals. Our near vision gradually declines, requiring stronger and stronger reading prescriptions, until around age 60 when the lens finally runs out of all flexibility, at which point our near prescription usually stabilizes. Presbyopia happens to everybody, and can occur with or without nearsightedness, farsightedness, and/or astigmatism. Presbyopic patients are also able to wear contact lenses to correct this “birthday-related” condition.